[ad_1]
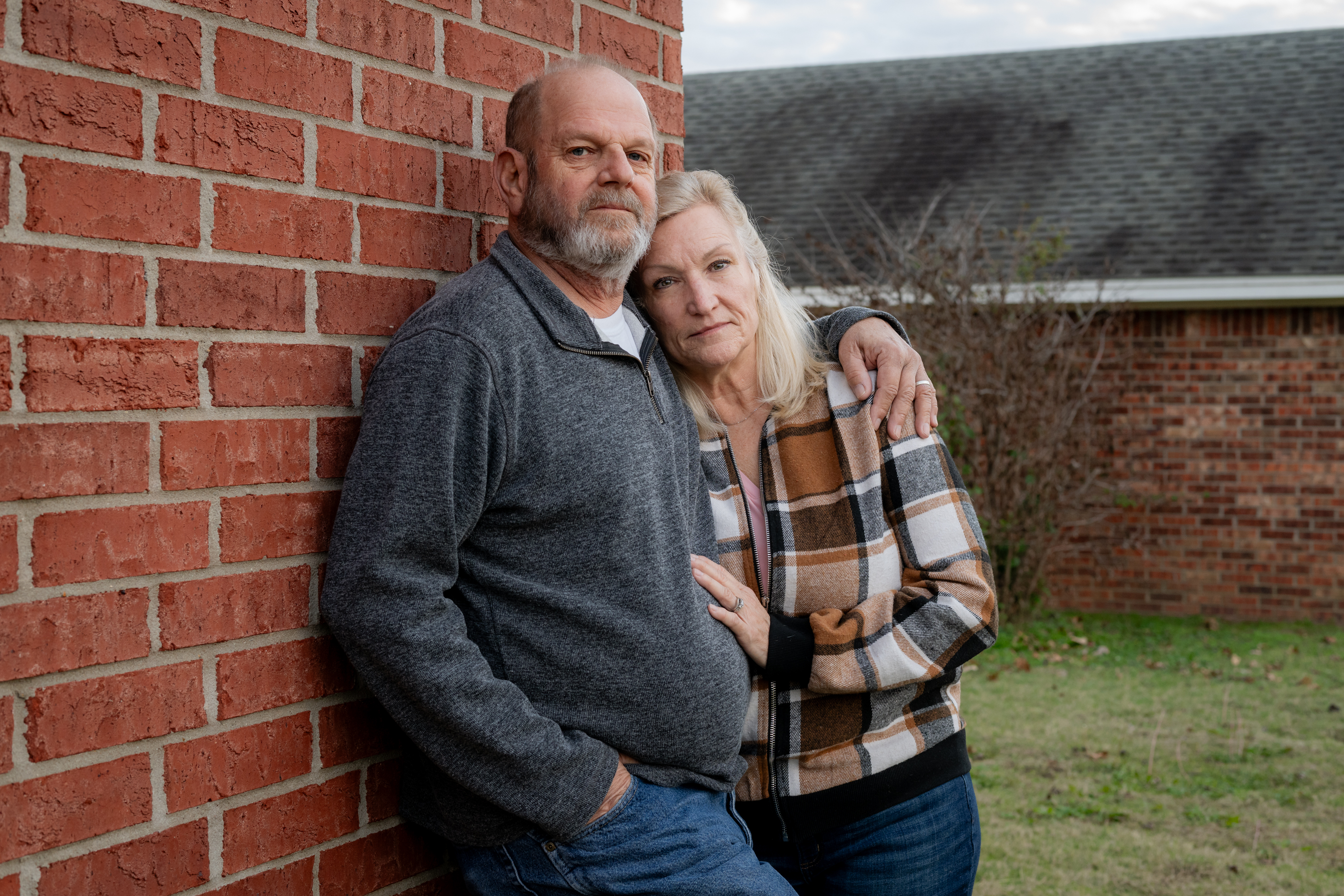
Marine Corps veteran Ron Winters clearly recollects his physician’s sobering evaluation of his bladder most cancers prognosis in August 2022.
“That is unhealthy,” the 66-year-old Durant, Oklahoma, resident remembered his urologist saying. Winters braced for the struggle of his life.
Little did he anticipate, nevertheless, that he wouldn’t be waging battle solely towards most cancers. He additionally was up towards the Division of Veterans Affairs, which Winters blames for dragging its ft and organising obstacles which have delayed his therapies.
Winters didn’t endure most cancers remedy at a VA facility. As a substitute, he sought care from a specialist by way of the Veterans Well being Administration’s Neighborhood Care Program, established in 2018 to boost veterans’ selections and scale back their wait occasions. However he stated the prior authorization course of was a chronic nightmare.
“For them to take weeks — as much as months — to offer an authorization is ridiculous,” Winters stated. “It doesn’t matter if it’s most cancers or not.”
After his preliminary prognosis, Winters stated, he waited 4 weeks for the VA to approve the process that allowed his urologic oncologist on the College of Texas Southwestern Medical Middle in Dallas to take away a number of the most cancers. Then, when he completed chemotherapy in March, he was pressured to attend one other month whereas the VA thought-about approving surgical procedure to take away his bladder. Even routine imaging scans that Winters wants each 90 days to trace progress require preapproval.
In a written response, VA press secretary Terrence Hayes acknowledged {that a} “delay in care is rarely acceptable.” After KFF Well being Information inquired about Winters’ case, the VA started working with him to get his ongoing care licensed.
“We may also urgently evaluation this matter and take steps to make sure that it doesn’t occur once more,” Hayes instructed KFF Well being Information.
Prior authorization isn’t distinctive to the VA. Most personal and federal medical insurance packages require sufferers to safe preapprovals for sure therapies, assessments, or prescription drugs. The method is meant to scale back spending and keep away from pointless, ineffective, or duplicative care, though the diploma to which firms and companies set these guidelines varies.
Insurers argue prior authorization makes the U.S. well being care system extra environment friendly by slicing waste — theoretically a win for sufferers who could also be harmed by extreme or futile remedy. However critics say prior authorization has turn out to be a instrument that insurers use to limit or delay costly care. It’s an particularly alarming situation for folks recognized with most cancers, for whom immediate remedy can imply the distinction between life and dying.
“I’m fascinated by worth and affordability,” stated Fumiko Chino, a member of the Affordability Working Group for the Memorial Sloan Kettering Most cancers Middle. However the best way prior authorization is used now permits insurers to implement “denial by delay,” she stated.
Most cancers is likely one of the most costly classes of illness to deal with within the U.S., in keeping with the Facilities for Illness Management and Prevention. And, in 2019, sufferers spent greater than $16 billion out-of-pocket on their most cancers remedy, a report by the Nationwide Most cancers Institute discovered.
To make issues worse, many most cancers sufferers have had oncology care delayed due to prior authorization hurdles, with some going through delays of greater than two weeks, in keeping with analysis Chino and colleagues revealed in JAMA in October. One other latest examine discovered that main insurers issued “pointless” preliminary denials in response to imaging requests, most frequently in endocrine and gastrointestinal most cancers circumstances.
The federal authorities is weighing new guidelines designed to enhance prior authorization for tens of millions of individuals coated by Medicare, Medicaid, and federal market plans. The reforms, if applied, would shorten the interval insurers are permitted to think about prior authorization requests and would additionally require firms to offer extra info once they situation a denial.
Within the meantime, sufferers — a lot of whom are going through the worst prognosis of their lives — should navigate a system marked by roadblocks, pink tape, and appeals.
“That is merciless and strange,” stated Chino, a radiation oncologist. A two-week delay may very well be lethal, and that it continues to occur is “unconscionable,” she stated.
Chino’s analysis has additionally proven that prior authorization is instantly associated to elevated anxiousness amongst most cancers sufferers, eroding their belief within the well being care system and losing each the supplier’s and the affected person’s time.
Leslie Fisk, 62, of New Smyrna Seaside, Florida, was recognized in 2021 with lung and mind most cancers. After seven rounds of chemotherapy final yr, her insurance coverage firm denied radiation remedy advisable by her medical doctors, deeming it medically pointless.
“I bear in mind dropping my thoughts. I want this radiation for my lungs,” Fisk stated. After preventing Florida Well being Care Plans’ denial “tooth and nail,” Fisk stated, the insurance coverage firm relented. The insurer didn’t reply to requests for remark.
Fisk referred to as the entire course of “horribly traumatic.”
“You need to navigate probably the most difficult system on the planet,” she stated. “Should you’re simply sitting there ready for them to maintain you, they gained’t.”
A new KFF report discovered that sufferers who’re coated by Medicaid seem like notably impacted by prior authorization, no matter their well being issues. About 1 in 5 adults on Medicaid reported that their insurer had denied or delayed prior approval for a remedy, service, go to, or drug — double the speed of adults with Medicare.
“Shoppers with prior authorization issues are likely to face different insurance coverage issues,” reminiscent of bother discovering an in-network supplier or reaching the restrict on coated providers, the report famous. They’re additionally “much more more likely to expertise severe well being and monetary penalties in comparison with folks whose issues didn’t contain prior authorization.”
In some circumstances, sufferers are pushing again.

In November, USA At present reported that Cigna admitted to creating an error when it denied protection to a 47-year-old Tennessee girl as she ready to endure a double-lung transplant to deal with lung most cancers. In Michigan, a former medical insurance government instructed ProPublica that the corporate had “crossed the road” in denying remedy for a person with lymphoma. And Blue Cross and Blue Defend of Louisiana “met its match” when the corporate denied a Texas trial lawyer’s most cancers remedy, ProPublica reported in November.
Numerous others have turned to social media to disgrace their medical insurance firms into approving prior authorization requests. Laws has been launched in at the least 30 states — from California to North Carolina — to handle the issue.
Again in Oklahoma, Ron Winters remains to be preventing. Based on his spouse, Teresa, the surgeon stated if Ron might have undergone his operation sooner, they may have prevented eradicating his bladder.
In some ways, his story echoes the nationwide VA scandal from almost a decade in the past, through which veterans throughout the nation had been languishing — some even dying — as they waited for care.
In 2014, for instance, CNN reported on veteran Thomas Breen, who was stored ready for months to be seen by a physician on the VA in Phoenix. He died of stage 4 bladder most cancers earlier than the appointment was scheduled.
Winters’ most cancers has unfold to his lungs. His prognosis has superior to stage 4.
“Actually, nothing has modified,” Teresa Winters stated. “The VA’s processes are nonetheless damaged.”
Do you will have an expertise with prior authorization you’d wish to share? Click on right here to inform your story.
[ad_2]