[ad_1]
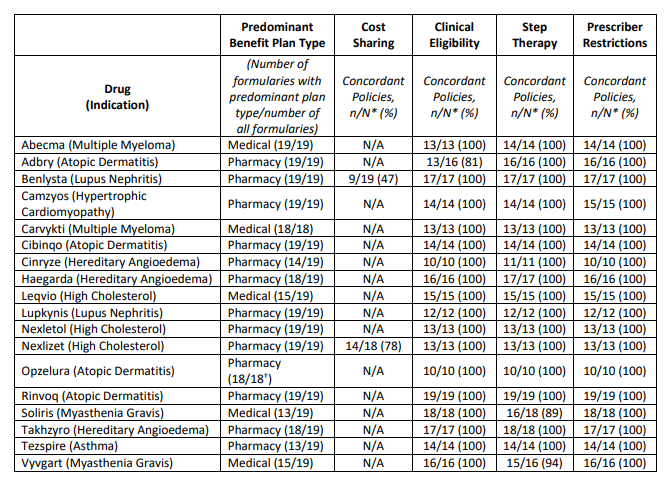
Final month, ICER launched their 2023 “Evaluation of Obstacles to Honest Entry” . The report concludes the next concerning 18 medication evaluated.
ICER defines “truthful entry” primarily based on the next standards:
Price sharing
- Price sharing primarily based on web value. Affected person price sharing ought to be primarily based on the web value to the plan sponsor, not the unnegotiated record value.
- No price for top worth therapies. All drugs recognized by the Inside Income Service as high-value therapies ought to obtain pre-deductible protection inside excessive deductible well being plans.
- One low-cost possibility obtainable in every class. At the very least one drug in each class ought to be coated on the lowest related cost-sharing stage except all medication are priced larger than a longtime truthful worth threshold.
- Okay to have excessive price sharing if no medication are cost-effective. If all medication in a category are priced so that there’s not a single drug that represents a good worth as decided by way of worth evaluation, it’s cheap for payers to have all medication on the next costsharing stage.
- If all medication are priced at truthful worth, formulary placement is appropriate. If all medication in a category are priced in order that they signify a good worth, it stays cheap for payers to make use of preferential formulary placement with tiered price sharing to assist obtain decrease total prices.
- Restricted cost-sharing if step-through required. As a part of financial step remedy, when sufferers strive a decrease price possibility with a decrease cost-sharing stage however don’t obtain an ample scientific response, price sharing for additional therapies also needs to be on the decrease cost-sharing stage so long as these additional therapies are priced pretty based on clear standards.
Though ICER record six standards, solely three (#3, #4, and #5) are formally assessed of their report.
Medical eligibility
- Payers ought to provide alternate options to prior authorization protocols equivalent to packages that give suggestions on prescribing patterns to clinicians or exempt them from prior authorization necessities (“gold carding”) in the event that they exhibit excessive constancy to evidence-based prescribing.
- Payers ought to doc a minimum of as soon as yearly that scientific eligibility standards are primarily based on prime quality, up-to date proof, with enter from clinicians with expertise in the identical or related scientific specialty.
- Medical eligibility standards ought to be developed with specific mechanisms that require payer workers to doc that they’ve: (i) thought-about limitations of proof on account of systemic under-representation of minority populations; and (ii) sought enter from scientific specialists on whether or not there are distinctive advantages and harms of remedy that will come up for organic, cultural, or social causes throughout totally different communities; and (iii) confirmed that scientific eligibility standards haven’t gone past cheap use of scientific trial inclusion/exclusion standards to interpret or slim the FDA label language in a approach that disadvantages sufferers with underlying disabilities unrelated to the situation being handled
- For all medication: Medical eligibility standards that complement the FDA label language could also be used to: (i) set requirements for analysis; and/or • Outline indeterminate scientific phrases within the FDA label (e.g., “moderate-to-severe”) with specific reference to scientific tips or different requirements; and/or (ii) triage sufferers by scientific acuity when the payer explicitly paperwork that triage is each cheap and needed
- For medication with costs or value will increase which have been deemed cheap: Apart from the three functions outlined above, scientific eligibility standards shouldn’t deviate from the FDA label language in a fashion that would chop protection.
- For medication with costs or value will increase which have been deemed cheap: Documentation that sufferers meet scientific eligibility standards ought to signify a light-weight administrative burden, together with acceptance of clinician attestation in lieu of extra formal medical document documentation except documentation is crucial to make sure affected person security.
- For medication with costs or value will increase which have been deemed unreasonable: Medical eligibility standards might slim protection by making use of particular eligibility standards from the pivotal trials used to generate proof for FDA approval if applied with cheap flexibility and supported by sturdy appeals procedures as described within the implementation standards.
Step Remedy and Switching
- As a way to justify financial step remedy insurance policies extending past FDA labeling as acceptable, payers ought to explicitly affirm or current proof to doc all the following: • Use of the first-step remedy reduces total well being care spending, not simply drug spending
- The primary-step remedy is clinically acceptable for all or almost all sufferers and doesn’t pose a larger threat of any vital aspect impact or hurt.
- Sufferers could have an affordable probability to fulfill their scientific objectives with first-step remedy.
- Failure of the first-step drug and the ensuing delay in starting the second-step agent won’t result in long-term hurt for sufferers.
- Sufferers should not required to retry a first-line drug with which they’ve beforehand had opposed unwanted effects or an insufficient response at an affordable dose and period.
- As a way to justify required switching insurance policies as acceptable, payers ought to explicitly affirm or current proof to doc all the following: (i) use of the required drug reduces total well being care spending. (ii) the required swap remedy is predicated on the identical mechanism of motion or presents a comparable threat and aspect impact profile to the index remedy. (iii) the required swap remedy has the identical route of administration or the distinction in route of administration will create no vital destructive influence on sufferers on account of scientific or socio-economic components. and (iv) sufferers should not required to change to a drug that they’ve used earlier than at an affordable dose and period with insufficient response and/or vital unwanted effects, together with earlier use underneath a distinct payer
Supplier {qualifications}
- Restrictions of protection to specialty prescribers are cheap with a number of of the next justifications: Ii) correct analysis and prescription require specialist coaching, with the danger that non-specialist clinicians would prescribe the treatment for sufferers who might undergo hurt or be unlikely to profit. (ii) willpower of the dangers and advantages of remedy for particular person sufferers requires specialist coaching on account of potential for critical unwanted effects of remedy. (iii) dosing, monitoring for unwanted effects, and total care coordination require specialist coaching to make sure secure and efficient use of the treatment.
- Requiring that non-specialist clinicians attest they’re caring for the affected person in session with a related specialist is an affordable possibility when the situation is ceaselessly handled in main care settings however some parts of dosing, monitoring for unwanted effects, and/or total coordination of care would profit from specialist enter for a lot of sufferers
Honest Entry Standards
- Price-sharing insurance policies ought to be introduced clearly to customers previous to well being plan choice, permitting all people to grasp what price sharing they’ll face for therapies they’re at present taking or are contemplating.
- Any vital change to formulary or price sharing buildings shouldn’t happen mid-cycle except plan sponsors embody this as a qualifying occasion permitting plan enrollees to change plans.
- On the level of care, clinicians and sufferers ought to have the ability to quickly decide the cost-sharing necessities for any remedy together with price sharing for different alternate options.
- People contemplating well being plan enrollment ought to be introduced with clear info permitting them to grasp whether or not they meet the insurers’ scientific standards for the therapies they’re at present taking. The insurance policies also needs to set out the rationale behind them and be readily comprehensible.
- Clinicians and sufferers ought to have the ability to quickly decide the scientific standards for any remedy and examine the scientific rationale supporting these standards. The referenced scientific info ought to be available to the prescribing/ordering supplier and the general public.
- People contemplating well being plan enrollment ought to be introduced with clear info permitting them to grasp whether or not the therapies they at present take or envision taking will probably be topic to non-medical step remedy or switching insurance policies.
- Clinicians, pharmacists, and sufferers ought to have the ability to quickly decide the necessities associated to step remedy and switching insurance policies and have the ability to simply view a full justification from the insurer.
- People contemplating well being plan enrollment ought to have the ability to simply discover info associated to protection standards, together with prescriber {qualifications}, for medication that they or members of the family are at present taking.
- Clinicians and sufferers ought to have the ability to quickly decide whether or not there’s a restriction on prescribing for any remedy. Insurers ought to present prepared help to main care clinicians looking for reference to a related specialist for session as wanted
You possibly can learn the total report right here.
[ad_2]