[ad_1]
Which may be the case. Trendy Healthcare experiences:
Final month, St. Charles Well being System threatened to chop ties with all Medicare Benefit plans subsequent 12 months, a transfer that would go away an estimated 26,000 native beneficiaries with out entry to a hospital lower than 100 miles away.
“The truth of Medicare Benefit in central Oregon is that it simply hasn’t lived as much as the promise,” St. Charles Well being System CEO Dr. Steve Gordon wrote in a information launch on the time. “A program meant to advertise seamless and better high quality care has as an alternative develop into a fragmented patchwork of administrative delays, denials and frustrations,” he stated. The Bend-based nonprofit firm declined to make an government out there for an interview.
St. Charles Well being System isn’t the one one. The article goes on to say that rural hospitals are “disproportionately affected by elements corresponding to reimbursement cuts or denied and delayed funds from Medicare Benefit plans as a result of Medicare enrollees make up most of their affected person populations.”
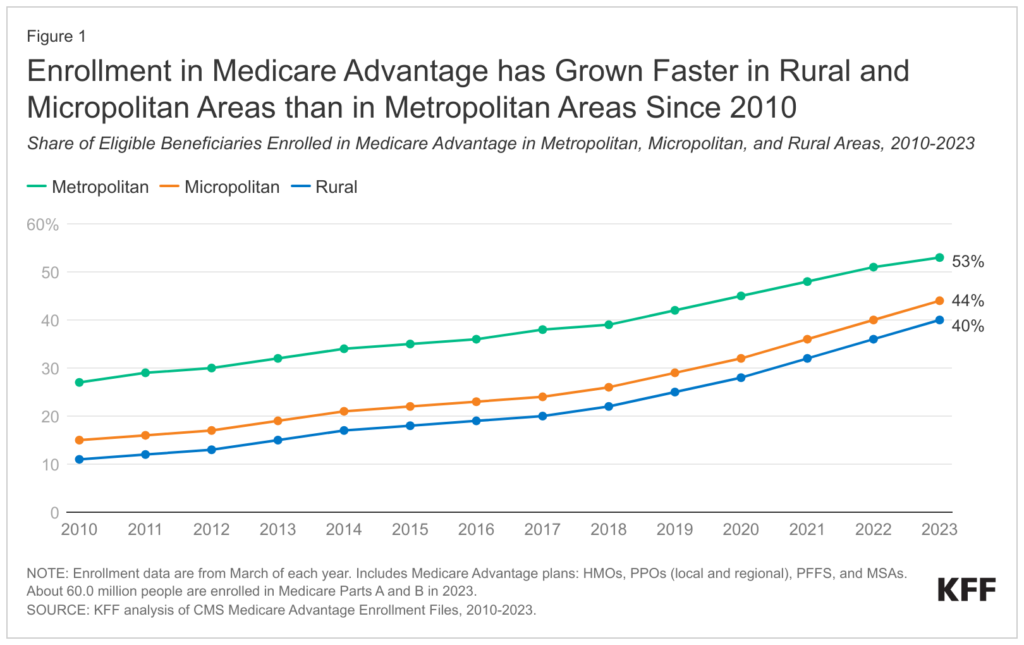
Rural hospitals are significantly delicate as a result of enrollment in Medicare Benefit amongst rural beneficiaries has grown from 11% to 40% of all rural Medicare beneficiaries between 2010 and 2023.
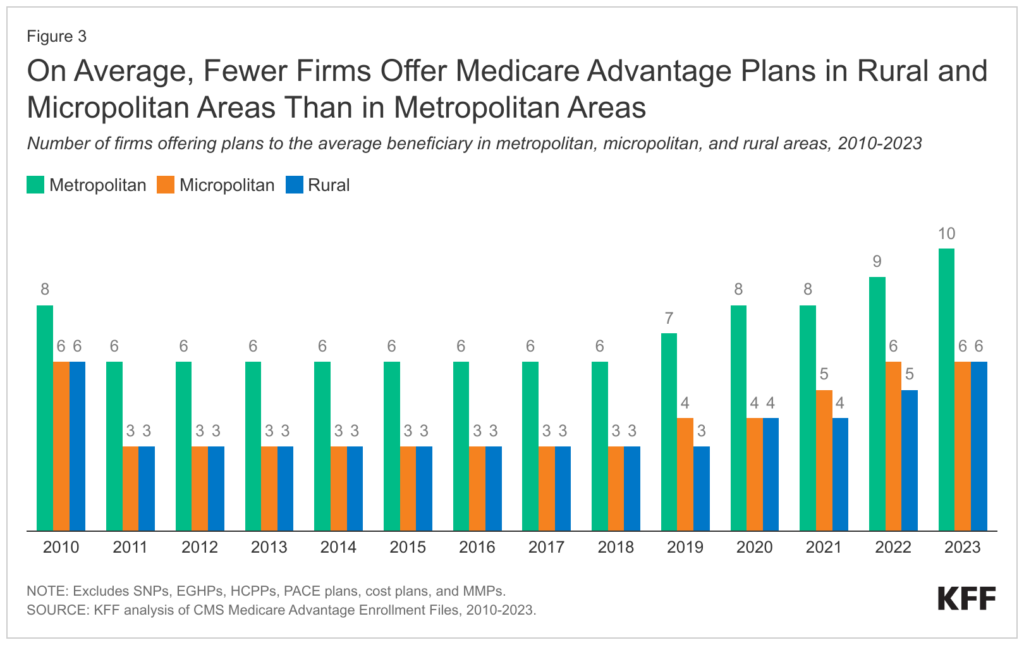
On the constructive facet, plan selection for rural Medicare Benefit beneficiaries has elevated, however this competitors has lead MA plans to intention to decrease premiums and go by way of these decrease prices to hospitals with decrease reimbursement and reimbursement delays.
My FTI Consulting colleague Adam Broder was additionally cited within the article, stating:
“It’s like, ‘What’s the purpose of preventing about charges if we are able to’t even receives a commission?’” Broder stated. “They earn a living on the business contracts. The margins are simply a lot smaller from Medicaid or Medicare, and if they will’t receives a commission on time or correctly or within the full quantity, then that’s going to result in a dispute.”
[ad_2]